QuickLinks
As we age, fine lines, wrinkles, age spots, and sun damage start to make themselves known on our skin. That’s where laser skin resurfacing at Dr. Andrews Plastic Surgery comes in. We offer a number of different types of laser therapy to ensure you get the customized treatment that addresses your concerns and achieves your desired results.
What is Laser Skin Resurfacing?
Laser skin resurfacing is often used to reduce facial wrinkles, scars, sun-damaged skin, and blemishes. The laser device sends short pulsating beams of light to the treatment area. But there isn’t only one type of laser skin resurfacing. There are a few different kinds, including ablative and nonablative.
The ablative laser removes the outermost layer of skin and heats the layer underneath to stimulate collagen production to improve the firmness and texture of your skin. The ablative laser treatment we provide is CO2 laser therapy.
The nonablative laser is less aggressive than the ablative option. The nonablative options include BBL (Broadband Light).
Both offer significant results, but ablative laser therapy has a longer recovery time.
Who is a Good Candidate for Laser Skin Resurfacing?
You may be a good candidate for laser skin resurfacing if you’re in generally good health, have realistic expectations, and have one or more of the following skin concerns:
- Fine lines and wrinkles
- Acne scars
- Hyperpigmentation
- Age spots
- Sun-damaged skin
If you have active acne, sagging or loose skin, and/or deep wrinkles, you are likely not a good candidate for laser skin resurfacing.
The Laser Skin Resurfacing Procedure
Laser skin resurfacing is an outpatient procedure and typically takes between 30 minutes and two hours. It depends on the size of the treatment area and the type of laser treatment you’re having done.
If you’re having ablative CO2 laser skin resurfacing done, an anesthetic will likely be applied to the skin to help with any discomfort.
For the CO2 laser resurfacing, the laser device will deliver laser energy and heat to the treatment area to remove thin layers of the outermost skin. By eliminating the top layer of the skin and penetrating deep within, collagen production increases, the body’s natural healing process goes into effect, and the skin is tightened and toned, providing dramatic results.
BBL, on the other hand, uses a broad-spectrum light to heat and penetrate the skin. This triggers the body’s natural healing process and stimulates collagen growth, reducing the appearance of pigmentation, and fine lines and wrinkles. Because no skin is removed, there is a shorter recovery time, but the results can be less noticeable.
Once your laser skin resurfacing is done, Dr. Andrews will apply a special dressing to the treatment area to ensure it’s protected.
Recovery
After treatment, you will likely see some redness and swelling. You may also experience some itching or stinging for the first few days. It may look like a moderate to severe sunburn, depending on the type of laser therapy you have.
For BBL treatment, your skin may become dry and start peeling after about a week.
For CO2 laser skin resurfacing, the recovery time is longer, and you may not see final improvements for several months. For the first few days, you will likely feel some discomfort, but it should resolve within 48 hours. For three to four days after treatment, your face will feel tight and swollen, and a crust may form. This is completely normal. As you heal, it will diminish, and your new brilliant skin will start to shine through. After about ten days, you should be mostly healed, but you may continue to see improvements for several more months.
No matter the type of laser therapy you have you’ll want to take proper care of your skin as it heals. To ensure proper healing and optimal results, you’ll want to avoid picking at your skin, clean the treated areas as advised, and wear protective skincare, including moisturizer and sunscreen. Try to minimize your level of sun exposure as much as possible for the first few months after treatment.
The results for BBL typically last for months and require repeated treatment to maintain those results. For CO2 laser therapy, the results can last for years.
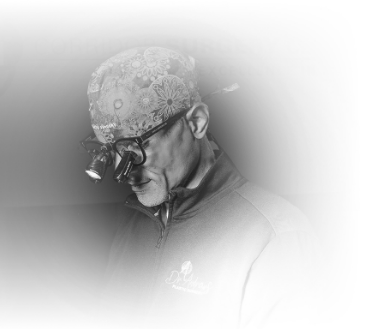
DR. KAHLIL ANDREWS
Dr. Kahlil Andrews is a board-certified plastic surgeon from Los Angeles specializing in plastic, cosmetic and reconstructive surgery.
At his location in Coralville, Iowa, Dr. Andrews’ academic and technical achievements are only exceeded by his commitment to patient care. Whether they are seeking reconstructive breast surgery, outpatient injectable treatment, or a full-blown mommy makeover, Dr. Andrews gives his full attention and focus on achieving excellent patient outcomes.
MEET DR. ANDREWSTestimonials
“Schedule A Consultation
Are you ready to achieve clear and more radiant skin? Laser skin resurfacing can transform your skin, providing you with a younger-looking appearance after only one treatment.
To learn more, schedule a consultation at Dr. Andrews Plastic Surgery today. Call our Coralville, IA office at (319) 800-6877 or use our online contact form.







